About the Author: Eric Bowman is a Registered Physiotherapist in Ontario, Canada who works in the areas of orthopedic physical therapy and exercise for people with chronic diseases. He’s also intermittently involved with the University of Waterloo Kinesiology program and the Western University Physical Therapy program. He also competes as a powerlifter in the Canadian Powerlifting Union and has completed the CPU Coaching Workshop & Seminar.
This past weekend (as of the time I’m writing this on a train to Toronto), Coach Travis Mash and I had a discussion regarding options for hip osteoarthritis (OA) and whether hip resurfacing, hip replacements, or stem cells would be the best option. It’s an understandable question given that OA is one of the two big musculoskeletal pain problems in today’s society (along with low back pain) and, given the aging of the baby boomers, it’s expected that these will rise.
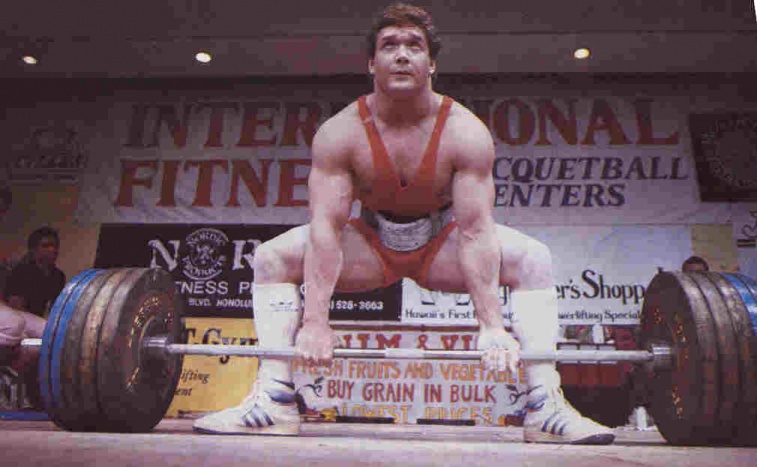
Serious athletes aren’t immune from this either. A recent paper showed that competitive runners were actually at a higher risk of developing OA than sedentary individuals. Heavy athletes (such as powerlifters, strongman, football players and bodybuilders) are at a higher risk of OA even when generally healthy.
It’s impossible for me to make recommendations for each individual with hip pain and hip OA without assessing them and understanding their situation. That said – people need to know the risks and benefits of the different, more invasive, options for hip OA.
First Things First: Conservative Options
I’d be crazy if I didn’t first recommend the simple steps for helping with hip OA which can greatly improve symptoms and have considerably lower risk compared to the options which I will discuss later on the article. The more conservative options include:
- Losing weight: Increased body weight is a big risk factor for OA, and some research has shown that losing weight is associated with improved pain and symptoms. If you’re considerably overweight and unhealthy, working with a doctor and a certified exercise physiologist (through ACSM or CSEP) is a good start to improving your symptoms.
- General strengthening of the hip, thigh, and core muscles: Powerlifters and weightlifters are pretty good with strengthening the quads, hamstrings, and glute max muscles as they are the ones that contribute to success in the squat, deadlift, snatch, and clean and jerk. But in many weight training clientele I’ve worked with, the abductors (i.e. glutes medius & minimus), adductors, and hip rotator muscles tend to be neglected. Strength athletes (with the exception of strongman) tend to train only in one plane of motion. If you aren’t training all of your hip and your core muscles, that’s another vital step that may improve your symptoms. Worse comes to worse – you’re better off coming out of the surgery.
- Improving sleep: Poor sleep can be a risk factor for a lot of different musculoskeletal pain conditions and for chronic pain. Some simple steps you can to improve your sleep are:
- Going to bed and getting up at the same time every night
- Limiting (if not eliminating) caffeine and alcohol use after lunchtime
- Minimizing screentime before bed (I’m a bit of a hypocrite and struggle with this part)
- Making sure the environment is cool, dark, and quiet
If you find these steps aren’t helping your quality of sleep, I recommend you get a sleep study – especially given the amount of bigger athletes who have sleep apnea and rely on CPAP machines.
- Managing psychosocial factors like stress, anxiety, and depression: these are major risk factors for chronic pain and poor recovery. I’m not a doctor (nor did I stay at a Holiday Inn Express last night) – but if simple steps such as eating right, exercising regularly, sleeping well, and better time management/organization aren’t helping … then it’s worth seeking out professional counseling or help to deal with these issues.
[thrive_leads id=’9063′]
Now with that out of the way, it’s time to answer Travis’s question: hip replacement vs hip resurfacing vs stem cell therapy – which is the best option?
Stem Cell Therapy
I could only find two human studies on PubMed which totaled 28 participants who were undergoing stem cell therapy for OA of the hip. These studies showed a slight improvement in pain with no complications.
As a disclaimer these studies were done in very small populations and research is needed to determine how long these effects last. My personal (anecdotal) bias and observations of any kind of cell injection are that many of them have shorter lasting effects in people.
Hip Resurfacing vs Hip Replacement
This area has been much more thoroughly researched and is an area I have considerably more experience with through doing a placement/internship at University Hospital in London, Canada. There I saw numerous clients post hip replacement (total hip arthroplasty) and resurfacing from surgery to discharge. I’ve seen the surgery done in person and have gotten to meet some of the surgeons involved in the practice guidelines surrounding THAs.
In terms of short term outcomes, some research has shown advantages of hip resurfacing over hip replacements, such as:
- Less pain 24 hours post-surgery
- Shorter hospital stay (by about 2 days on average)
- Less blood loss and transfusions
- Lower rate of hip dislocations
In terms of overall pain and functional outcomes, aside from a few odd questionnaires here
and there, the outcomes for pain and physical function are generally the same between the two
surgeries.
The big advantage of hip replacement over hip resurfacing is that the implements last longer and need less revision.
In my experience, and the research says this, the vast majority of people do quite well after a hip replacement … and the anterior hip replacement approach has good evidence when compared to the lateral and approaches. The people whom I see struggle are:
- People who have let themselves go and are incredibly obese, weak, and/or inflexible heading into surgery.
- Those who don’t do their exercises and/or are afraid of moving the operated hip for fear of pain or damage.
- People who unfortunately suffer from central sensitization, a condition in which the entire nervous system and body is hypersensitive and produces excess levels of pain in response to stimuli. These are examples of people where a more generalized approach focusing not just on exercise or surgery but on general health (i.e. diet, sleep, stress, beliefs) can be necessary and essential.
Again – it’s impossible for me to make specific recommendations without knowing your situation, but I hope this provides some useful tips for future consideration. As always, thanks for reading.
References
Ortiz-Declet VR, Iacobelli DA, Yuen LC, Perets I, Chen AW, Domb BG. Birmingham Hip Resurfacing vs Total Hip Arthroplasty: A Matched-Pair Comparison of Clinical Outcomes. J Arthroplasty. 2017 Dec;32(12):3647-3651. doi: 10.1016/j.arth.2017.06.030. Epub 2017 Jun 23. PubMed PMID: 28711342.
Shimmin AJ, Baré JV. Comparison of functional results of hip resurfacing and total hip replacement: a review of the literature.Orthop Clin North Am. 2011 Apr;42(2):143-51, vii. doi: 10.1016/j.ocl.2010.12.007. Review. PubMed PMID: 21435490.
Alberta Hip Improvement Project., MacKenzie JR, O’Connor GJ, Marshall DA, Faris PD, Dort LC, Khong H, Parker RD, Werle JR, Beaupre LA, Frank CB. Functional outcomes for 2 years comparing hip resurfacing and total hip arthroplasty. J Arthroplasty. 2012 May;27(5):750-7.e2. doi: 10.1016/j.arth.2011.10.004. Epub 2012 Jan 28. PubMed PMID: 22285258.
Yoon RS, Geller JA, Nyce JD, Morrison TA, Macaulay W. Hip resurfacing is less painful at 24 hours than hip replacement.Orthop Clin North Am. 2012 Nov;43(5):e8-13. doi: 10.1016/j.ocl.2012.07.002. Epub 2012 Sep 8. PubMed PMID: 23102425.
Marshall DA, Pykerman K, Werle J, Lorenzetti D, Wasylak T, Noseworthy T, Dick DA, O’Connor G, Sundaram A, Heintzbergen S, Frank C. Hip resurfacing versus total hip arthroplasty: a systematic review comparing standardized outcomes. Clin Orthop Relat Res. 2014 Jul;472(7):2217-30. doi: 10.1007/s11999-014-3556-3. Epub 2014 Apr 4. Review. PubMed PMID: 24700446; PubMed Central PMCID: PMC4048407.
Emadedin M, Ghorbani Liastani M, Fazeli R, Mohseni F, Moghadasali R, Mardpour S, Hosseini SE, Niknejadi M, Moeininia F, Aghahossein Fanni A, Baghban Eslaminejhad R, Vosough Dizaji A, Labibzadeh N, Mirazimi Bafghi A, Baharvand H, Aghdami N. Long-Term Follow-up of Intra-articular Injection of Autologous Mesenchymal Stem Cells in Patients with Knee, Ankle, or Hip Osteoarthritis. Arch Iran Med. 2015 Jun;18(6):336-44. doi: 015186/AIM.003. PubMed PMID: 26058927.
Mardones R, Jofré CM, Tobar L, Minguell JJ. Mesenchymal stem cell therapy in the treatment of hip osteoarthritis. J Hip Preserv Surg. 2017 Mar 19;4(2):159-163. doi: 10.1093/jhps/hnx011. eCollection 2017 Jul. PubMed PMID: 28630737; PubMed Central PMCID: PMC5467400.
Issa K, Palich A, Tatevossian T, Kapadia BH, Naziri Q, Mont MA. The outcomes of hip resurfacing compared to standard primary total hip arthroplasty in Men. BMC Musculoskelet Disord. 2013 May 8;14:161. doi: 10.1186/1471-2474-14-161. PubMed PMID: 23656900; PubMed Central PMCID: PMC3652766.
Ward WG, Carter CJ, Barone M, Jinnah R. Primary total hip replacement versus hip resurfacing – hospital considerations.Bull NYU Hosp Jt Dis. 2011;69 Suppl 1:S95-7. PubMed PMID: 22035493.
Penny JØ, Ovesen O, Varmarken JE, Overgaard S. Similar range of motion and function after resurfacing large-head or standard total hip arthroplasty. Acta Orthop. 2013 Jun;84(3):246-53. doi: 10.3109/17453674.2013.788435. Epub 2013 Mar 26. PubMed PMID: 23530872; PubMed Central PMCID: PMC3715815.